Using the metaphor of a summer family road trip, Phil McClure, PT, PhD, FAPTA, said that a probing question still applicable to the concept of the movement system is, "Are we there yet?"
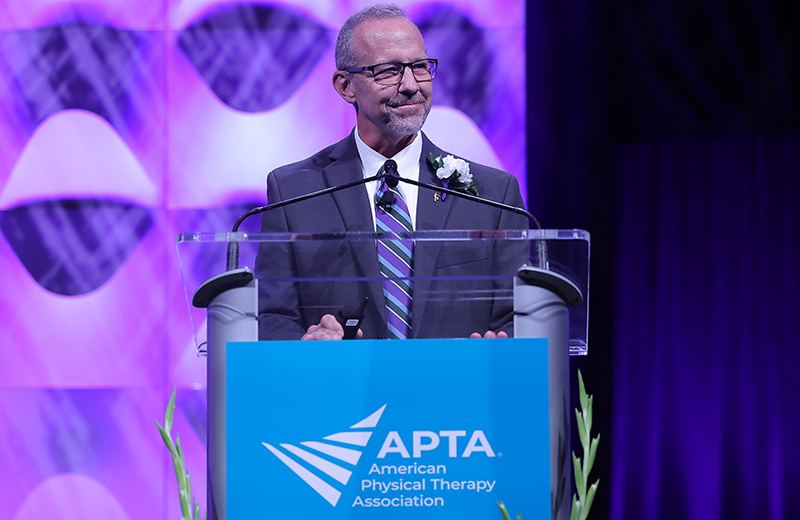
McClure, professor and chair of the Department of Physical Therapy at Arcadia University, delivered the 29th John H.P. Maley lecture on July 21 as part of the APTA Leadership Congress in Kansas City, Missouri.
Considering the profession's destination of transforming society by optimizing movement to improve the human experience, widespread consensus on two key topics — the movement system and diagnosis — has been slow, McClure said.
"We have a long history of struggling with professional identity, but movement has historically been at our professional core," he said.
McClure's lecture, titled "The Movement System and Diagnosis — Are We There Yet?" offered propositions that he believes could make the movement system more relevant and meaningful.
McClure had three frameworks to guide his presentation: defining the movement system, adopting the movement system as a foundational concept or model, and developing evidence-based diagnostic classification systems.
1. Creating an Operational Definition of the Movement System
In an informal survey of clinicians, McClure said he found there was no clear and unified understanding of the movement system.
At issue, McClure indicated, is that the term lacks an operational definition, making it difficult to translate into education and practice.
"If the movement system is to be our unique identity, we need to create and define a truly unique system and model that can be readily understood and distinguished from the expertise of other health professionals," McClure said.
That said, it's important to recognize that "physical therapists do not own the movement system," McClure said. "We must be leaders and experts around movement, but we must also collaborate and utilize expertise from others."
One barrier to such collaboration is terminology. "If we insist on highly nuanced and physical therapist-specific jargon, at best we will be isolated, and, at worst, we will become irrelevant," McClure said.
2. Isolating the Movement System as a Foundational Concept or Model
McClure's second proposal is to isolate the movement system as a foundational concept or model, independent of diagnostic classification schemes.
"The variety of patients and health conditions encountered by physical therapists and the specific nature of the contextual factors are simply too broad for a single comprehensive system to be meaningfully applied," McClure said.
Additionally, a hyper-focus on movement diagnoses inevitably prioritizes biological aspects of the biopsychosocial model of health, despite the growing evidence of the importance of psychological factors, he said.
"I believe a simpler and more straightforward approach is to isolate the movement system as a model explaining movement — period," he said.
Isolating the core elements of movement allows the profession to study movement as a defined phenomenon and understand the relationship between movement and outcomes such as pain and functional performance, McClure said.
3. Developing Diagnostic Classification Systems for the Movement System
McClure called for clinical scientists to develop meaningful diagnostic schemes, with associated tests and measures, that are tested for reliability and validity.
Specialty academies can guide this work, he added, and funders could support clinical research focused on these classifications in multidisciplinary research groups.
However, McClure cautioned, diagnostic labels are just one piece of health care.
"Do clinicians really rely on a diagnostic label to guide specific management of a patient?" he asked. "Capturing all relevant biopsychosocial aspects of a patient's health condition in a single label seems somewhat of a fool's errand. I would posit that effective and experienced clinicians, both physicians and therapists, would readily acknowledge that they consider many patient-specific factors not captured by a label to guide specific interventions."
When looking at the growth of the profession, it's important to look at which patients PTs and PTAs can most likely help. In other words, McClure said, where does the profession offer the most value in the system?
Developing a set of "appropriateness criteria" to help physicians understand which patients are most likely to be helped when referred to physical therapy could be an important achievement for the profession, he said.
"If it were developed by a multidisciplinary group in a way that could be defended and realistically accessed and implemented on a broad scale, it would provide a significant step forward towards value-based care," McClure said.